We have recently shown that XPO1 mutations are drivers of lymphomagenesis and occur across B-cell lymphomas, specifically in chronic lymphocytic leukemia (CLL), classical Hodgkin lymphoma and primary mediastinal B-cell lymphoma. The co-occurrence of other oncogenic events cooperating with XPO1 provides an opportunity for combined targeted therapy. Increased expression of the anti-apoptotic factor BCL2 has long been known to be a critical part of the pathophysiology of B-cell lymphomas. Recently, the oral BCL2 inhibitor, venetoclax, was approved in CLL and is currently being evaluated in clinical trials for other B-cell lymphomas. Selinexor is a potent, oral XPO1 inhibitor that was recently approved in multiple myeloma and diffuse large B-cell lymphoma. XPO1 inhibition exerts its antineoplastic effects by blocking key lymphomagenic pathways, such as NFκB, and decreasing the anti-apoptotic protein survivin. We therefore hypothesized that combining selinexor and venetoclax would have potential synergy and provide an oral precision combination therapy for relapsed, refractory lymphoma.
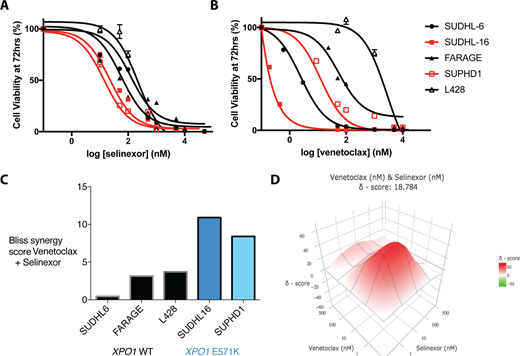
We first set out to determine whether XPO1 mutant lymphoma cell lines showed differential response to either selinexor or venetoclax monotherapy. Five lymphoma cell lines; 3 diffuse large B-cell lymphoma (SU-DHL-6, SU-DHL-16, FARAGE) and 2 classical Hodgkin lymphoma (L428 and SUP-HD1), were subjected to next-generation sequencing (NGS) to assess for the presence or absence of XPO1 mutations. SUDHL-16 and SUP-HD1 were heterozygous for the XPO1 E571K hotspot mutation while SUDHL-6, FARAGE and SUP-HD1 were wildtype at the XPO1 locus. These 5 cell lines were used to assess sensitivity to Selinexor and/or Venetoclax. The CellTiter Glo assay was used to assess cell viability after 72 hours of treatment. Assays were performed in triplicate on 96-well plates that were read using a Spectramax plate reader. The XPO1 mutant cells showed increased sensitivity to selinexor (XPO1 mutant IC50 = 16-35nM; XPO1 WT IC50 = 41-231nM) as previously seen in conditional knockin mouse models of XPO1 mutant CLL (Figure A). Additionally, the XPO1 mutant cell lines showed increased sensitivity to single-agent venetoclax (XPO1 mutant IC50 = 2-13nM; XPO1 WT IC50 = 5-2853nM), an observation that has not previously been made (Figure B).
Next, we tested the synergy of the combination of selinexor and venetoclax in the XPO1 mutant and wildtype cell lines. Increasing concentrations of the individual drugs were applied to each individual cell line in a 6x6 matrix. The cell viability percentage for each concentration was then entered into a synergy finder (www. synergyfinder.fimm.fi). The Bliss Independence model was used to calculate synergy of the Selinexor-Venetoclax combinations. As hypothesized, the combination of selinexor and venetoclax indeed showed synergy in both the wildtype and mutant XPO1 cell lines. Furthermore, the XPO1 mutant cell lines showed a higher degree of synergy compared to the wildtype cells (Figure C).
Finally, a remarkable patient allowed us to test this combination ex vivo. This patient with CLL had undergone multiple therapies including chemoimmunotherapy, ibrutinib and venetoclax monotherapies. This patient had a founder XPO1 E571K mutation and also had acquired a BTK C481S ibrutinib resistance mutation and MYC amplification. These cells were unique in that they were easily able to be tested in ex-vivo culture to test sensitivity to different therapies. When tested with chemotherapy or ibrutinib they were completely resistant, and even with venetoclax they were fairly resistant; however, they remained sensitive to XPO1 inhibition with Selinexor. Selinexor and venetoclax showed remarkable synergy measured by a BLISS delta score of 18.78 (Figure D).
In conclusion, inhibiting the nuclear exporter XPO1 and the anti-apoptotic factor BCL2 is synergistic in both XPO1 wildtype and mutant lymphoma. XPO1 mutant lymphomas show increased sensitivity to both selinexor and venetoclax. Additionally, selinexor and venetoclax showed a higher degree of synergism in XPO1 mutant lymphoma cell lines and were highly synergistic in primary XPO1 mutant CLL patient cells ex vivo. This combination is highly promising as an all oral alternative for relapsed, refractory lymphoma. Next steps include preclinical testing in mouse models in vivo using XPO1 mutant and wildtype mice crossed with mice overexpressing BCL2.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal